Curious if your nightly snores are just harmless noise or a sign of something more serious? Snoring and sleep apnea may seem similar, but they’re distinct sleep disturbances.
While snoring is often dismissed as a nuisance, sleep apnea involves potentially dangerous breathing interruptions.
Let’s explore into the crucial disparities between these two nighttime phenomena to unveil their impact on your health and sleep quality.
Table of Contents
Understanding the Connection Between Snoring and Sleep Apnea
A. What Causes Snoring?
Snoring is a common phenomenon that affects a significant portion of the population. It occurs when the airflow through the throat and nasal passages becomes obstructed during sleep, causing the soft tissues in the throat to vibrate. Several factors can contribute to the occurrence of snoring, including:
1. Exploring the Common Triggers of Snoring
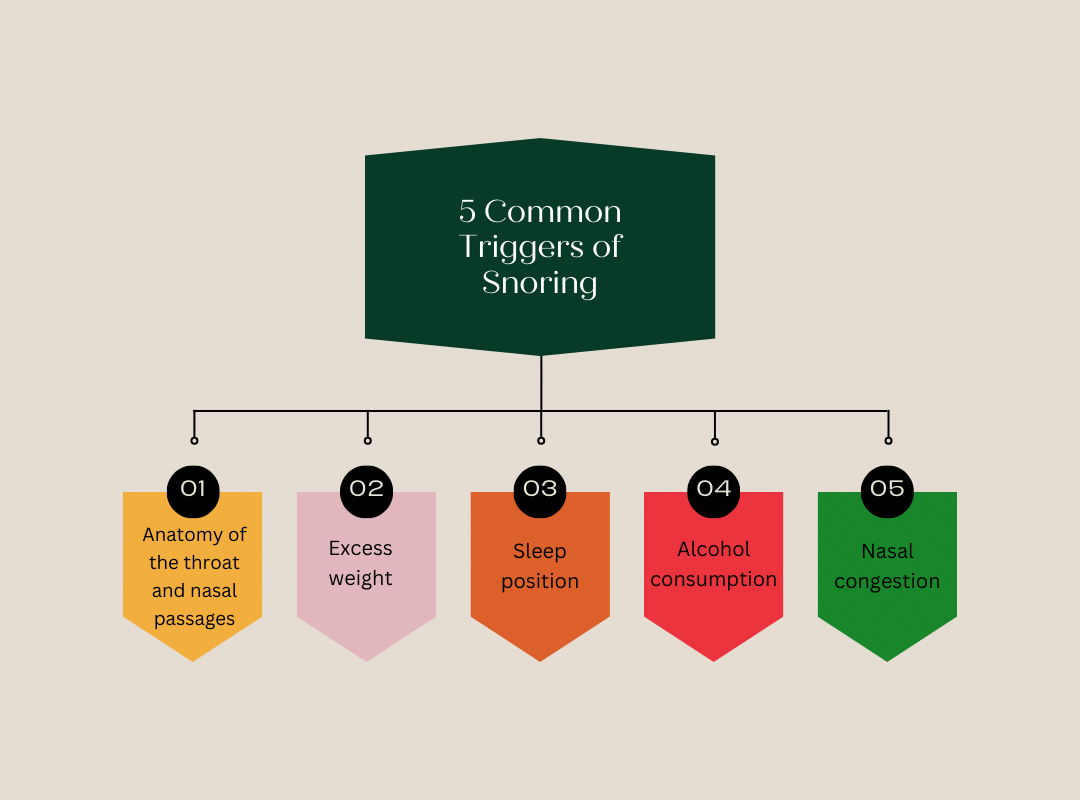
- Anatomy of the throat and nasal passages: Individuals with a narrow airway, large tonsils, or a long soft palate are more prone to snoring.
- Excess weight: Individuals who are overweight or obese often have excess tissue in the throat and neck, which can obstruct airflow and lead to snoring.
- Sleep position: Sleeping on one’s back can cause the tongue and soft palate to fall back into the throat, leading to snoring.
- Alcohol consumption: Consuming alcohol before bedtime can relax the throat muscles, exacerbating snoring.
- Nasal congestion: Conditions that cause nasal congestion, such as allergies or a deviated septum, can contribute to snoring.
2. Factors Contributing to Nocturnal Noise
In addition to the physical factors that can trigger snoring, certain lifestyle and environmental elements can also play a role in the intensity and frequency of snoring. These include:
- Age: Snoring tends to become more common as individuals age, as the throat muscles and tissues lose tone and flexibility.
- Gender: Men are more likely to snore than women, due to differences in muscle tone and body composition.
- Sleep position: Sleeping on one’s back can exacerbate snoring, while sleeping on one’s side may help reduce it.
- Fatigue and sleep deprivation: Lack of quality sleep can cause the muscles in the throat to relax more, leading to increased snoring.
- Medications: Certain medications, such as sedatives and muscle relaxants, can contribute to snoring by relaxing the throat muscles.
B. What Is Sleep Apnea?
1. Defining Sleep Apnea: Types and Symptoms
Sleep apnea is a sleep disorder characterized by recurrent pauses in breathing or shallow breathing during sleep. There are two main types of sleep apnea:
- Obstructive Sleep Apnea (OSA): This is the most common form of sleep apnea, occurring when the throat muscles relax and block the airway during sleep.
- Central Sleep Apnea (CSA): In this less common form, the brain fails to signal the muscles to breathe, leading to pauses in breathing.
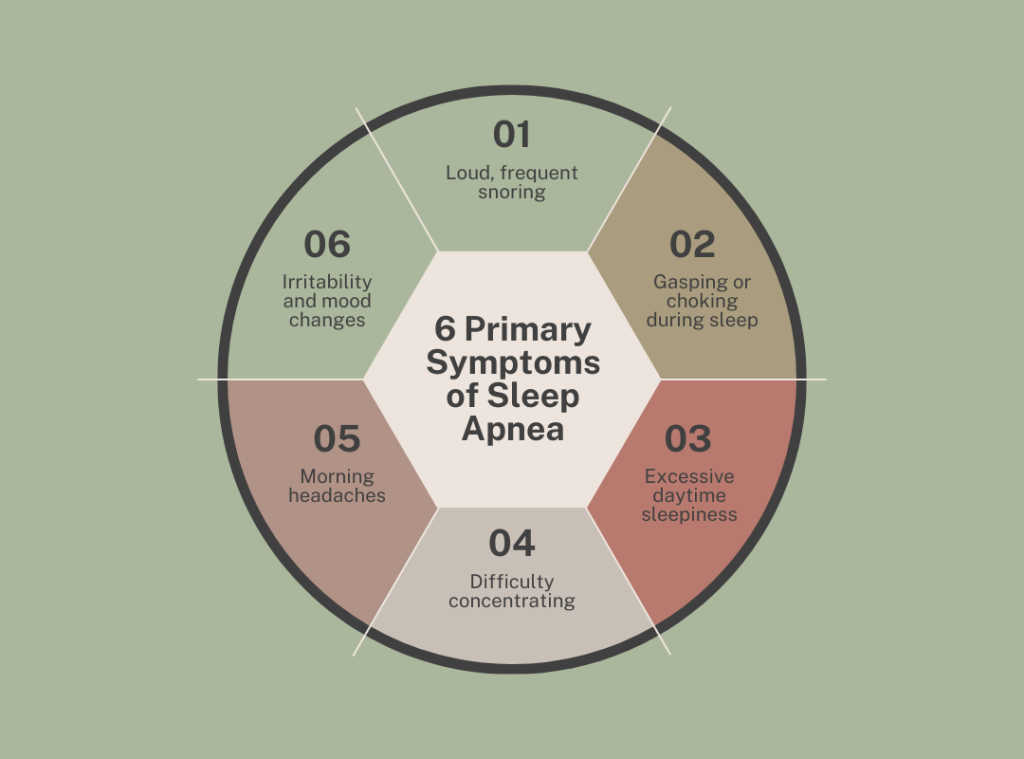
The primary symptoms of sleep apnea include:
2. Understanding the Mechanics of Sleep Disordered Breathing
During sleep, the muscles in the throat and neck relax, which can cause the airway to become partially or completely blocked. This blockage leads to a lack of oxygen and an accumulation of carbon dioxide in the bloodstream, triggering the brain to briefly wake the individual to resume normal breathing.
In the case of obstructive sleep apnea, this cycle of breathing interruptions and wakeups can occur dozens or even hundreds of times per night, preventing the individual from reaching the deep, restorative stages of sleep. This sleep fragmentation and oxygen deprivation can have significant consequences for the individual’s health and well-being.
Snoring vs. Sleep Apnea
A. Distinguishing Between Snoring and Sleep Apnea
While snoring and sleep apnea are related, they are not the same condition. Snoring is a common occurrence that affects many individuals, but it does not necessarily indicate the presence of sleep apnea. The key difference lies in the severity and impact of the breathing disruptions.
Snoring is the audible vibration of the soft tissues in the throat, often caused by the relaxation of the throat muscles during sleep. It is a relatively common phenomenon and, in many cases, does not significantly impact the individual’s health or sleep quality.
In contrast, sleep apnea is a more severe condition characterized by complete or partial airway blockages that lead to frequent breathing interruptions and disrupted sleep. These breathing pauses can have serious consequences for the individual’s overall health and well-being.
B. Recognizing the Telltale Signs of Each Condition
While snoring and sleep apnea share some common symptoms, there are distinct signs that can help distinguish between the two conditions:
Snoring:
- Loud, frequent snoring that may be disruptive to others
- Snoring that occurs in various sleep positions
- Snoring that does not significantly impact sleep quality or daytime functioning
Sleep Apnea:
- Loud, frequent snoring that is interrupted by pauses in breathing
- Gasping or choking sounds during sleep
- Excessive daytime sleepiness, despite adequate sleep time
- Difficulty concentrating or memory problems
- Morning headaches
- Irritability and mood changes
C. Indications That Snoring Might Be Sleep Apnea
1. Identifying Red Flags: When Snoring Signals a Larger Issue
While not all snoring is indicative of sleep apnea, there are certain red flags that may suggest the presence of a more serious sleep disorder:
- Loud, frequent snoring that is accompanied by pauses in breathing
- Excessive daytime sleepiness or fatigue despite adequate sleep time
- Witnessed episodes of breathing cessation or gasping during sleep
- Persistent, unexplained headaches upon waking
- Increased risk factors, such as obesity, large neck circumference, or a family history of sleep apnea
2. Understanding the Overlapping Symptoms
Snoring and sleep apnea share several common symptoms, including:
- Loud, disruptive snoring
- Daytime fatigue and sleepiness
- Difficulty concentrating or memory problems
- Morning headaches
However, the key distinction lies in the severity and impact of these symptoms. In sleep apnea, the breathing interruptions and sleep fragmentation can have more significant consequences for the individual’s health and well-being.
Health Ramifications of Snoring and OSA
A. Exploring the Impact on Overall Health and Well-being
Both snoring and obstructive sleep apnea (OSA) can have far-reaching consequences for an individual’s health and quality of life. While snoring may be a nuisance for both the individual and their sleeping partner, untreated OSA can lead to more severe health complications.
Chronic snoring, even in the absence of sleep apnea, has been linked to several health issues, including:
- Daytime fatigue and reduced productivity
- Increased risk of high blood pressure and heart disease
- Disrupted sleep for the individual and their sleeping partner
Obstructive sleep apnea, on the other hand, has been associated with a range of more serious health problems, such as:
- Cardiovascular disease, including high blood pressure, heart attacks, and strokes
- Metabolic disorders, including type 2 diabetes and obesity
- Neurological issues, including cognitive impairment and depression
- Respiratory problems, such as chronic obstructive pulmonary disease (COPD)
B. Long-Term Consequences of Untreated Sleep Disorders
Leaving snoring or sleep apnea untreated can have significant long-term consequences for an individual’s overall health and well-being. Over time, the chronic sleep disruption and oxygen deprivation associated with these conditions can contribute to the development of various health problems, including:
- Cardiovascular disease: Untreated sleep apnea can increase the risk of high blood pressure, heart attacks, and strokes.
- Metabolic disorders: Sleep apnea has been linked to an increased risk of type 2 diabetes and obesity.
- Neurological issues: Sleep disorders can impair cognitive function, increase the risk of depression, and contribute to the development of neurodegenerative diseases.
- Respiratory problems: Sleep apnea can exacerbate existing respiratory conditions, such as COPD, and increase the risk of respiratory failure.
- Accidents and injuries: Excessive daytime sleepiness associated with sleep apnea can increase the risk of accidents, both at home and on the road.
Early detection and proper management of snoring and sleep apnea are crucial to mitigate these long-term health consequences and improve the individual’s overall quality of life.
Factors that Affect Sleep Apnea
A. Examining the Influential Factors on Sleep Apnea Severity
- Anatomical factors:
- Narrowed airway: Individuals with a naturally smaller or narrower throat or nasal passage are more prone to experiencing airway obstruction during sleep.
- Excess weight and fat deposition: Overweight and obese individuals often have excess fat tissue around the neck and throat, which can contribute to airway constriction.
- Craniofacial structure: Certain facial and jaw abnormalities, such as a small lower jaw or a receding chin, can lead to a narrower airway and increase the risk of OSA.
- Enlarged tonsils or adenoids: Enlarged lymphoid tissues in the throat can partially block the airway, especially in children.
- Age and gender:
- Age: The risk of OSA increases with age, as the muscles in the throat and neck tend to lose tone and flexibility over time.
- Gender: Men are more prone to developing OSA compared to women, likely due to differences in body composition and muscle tone.
- Lifestyle factors:
- Obesity: Being overweight or obese is a significant risk factor for OSA, as excess body weight can contribute to airway obstruction.
- Alcohol consumption: Consuming alcohol before bedtime can relax the throat muscles, exacerbating airway blockage during sleep.
- Smoking: Cigarette smoking can cause inflammation and swelling in the upper airway, increasing the risk of OSA.
Understanding these influential factors can help healthcare providers better assess and manage the severity of an individual’s sleep apnea, leading to more effective treatment strategies.
B. Lifestyle Choices and Their Impact on Sleep Quality
In addition to the anatomical and medical factors that can affect sleep apnea severity, an individual’s lifestyle choices can also have a significant impact on their sleep quality and the progression of the condition.
- Weight management:
- Maintaining a healthy weight or losing excess weight can help reduce the severity of OSA by decreasing the amount of excess tissue around the neck and throat.
- Regular exercise and a balanced diet can be effective in managing weight and improving sleep apnea symptoms.
- Alcohol consumption:
- Avoiding or limiting alcohol intake, especially before bedtime, can help prevent the relaxation of the throat muscles and improve airflow during sleep.
- Smoking cessation:
- Quitting smoking can help reduce inflammation and swelling in the upper airway, which can contribute to improved breathing during sleep.
- Sleep position:
- Sleeping on one’s side rather than on the back can help prevent the tongue and soft palate from falling back into the throat, reducing the risk of airway obstruction.
- Stress management:
- Incorporating stress-reducing techniques, such as meditation, yoga, or relaxation exercises, can help improve overall sleep quality and potentially alleviate the severity of sleep apnea.
By making informed lifestyle choices, individuals with sleep apnea or at risk of developing the condition can take proactive steps to manage their symptoms and improve their overall sleep quality and health outcomes.
Treating Chronic Snoring

A. Strategies and Interventions for Managing Persistent Snoring
For individuals who experience chronic or persistent snoring, there are various strategies and interventions that can be employed to help manage the condition:
- Lifestyle modifications:
- Weight loss: Maintaining a healthy weight or losing excess weight can help reduce the amount of tissue around the neck and throat, improving airflow during sleep.
- Sleep position: Sleeping on one’s side rather than on the back can help prevent the tongue and soft palate from falling back into the throat, reducing snoring.
- Avoiding alcohol and sedatives: Abstaining from or limiting the consumption of these substances before bedtime can help prevent the relaxation of the throat muscles.
- Oral devices:
- Mandibular advancement devices (MADs): These custom-fitted mouthpieces gently hold the lower jaw forward, preventing the tongue and soft palate from obstructing the airway.
- Tongue-retaining devices: These devices hold the tongue in a forward position, keeping the airway open during sleep.
- Nasal devices:
- Nasal dilators: These small, external devices gently open the nostrils, improving airflow through the nasal passages.
- Nasal sprays or rinses: These can help reduce nasal congestion and improve breathing during sleep.
It’s important to note that the effectiveness of these interventions may vary, and healthcare providers can help determine the most suitable approach based on the individual’s specific condition and needs.
B. Lifestyle Modifications and Remedies for Better Sleep
In addition to targeted interventions, individuals with chronic snoring can also implement various lifestyle modifications and home remedies to improve their sleep quality and potentially reduce snoring:
- Weight management:
- Maintaining a healthy weight or losing excess weight can help reduce the amount of tissue around the neck and throat, improving airflow during sleep.
- Regular exercise and a balanced diet can be effective in managing weight and reducing snoring.
- Sleep position:
- Sleeping on one’s side rather than on the back can help prevent the tongue and soft palate from falling back into the throat, reducing snoring.
- Propping up the head with extra pillows or using a wedge pillow can also help keep the airway open.
- Nasal congestion relief:
- Using nasal sprays, rinses, or saline solutions can help reduce nasal congestion and improve breathing during sleep.
- Addressing underlying conditions, such as allergies or a deviated septum, can also help alleviate nasal obstruction.
- Avoiding alcohol and sedatives:
- Abstaining from or limiting the consumption of these substances before bedtime can help prevent the relaxation of the throat muscles and reduce snoring.
- Maintaining a consistent sleep schedule:
- Establishing a regular sleep-wake cycle and practicing good sleep hygiene can help improve the overall quality of sleep and potentially reduce snoring.
By implementing these lifestyle modifications and home remedies, individuals with chronic snoring may be able to achieve better sleep quality and potentially reduce the severity of their snoring without the need for more invasive interventions.
CPAP Therapy for Obstructive Sleep Apnea
A. Overview of Continuous Positive Airway Pressure (CPAP) Therapy
Continuous Positive Airway Pressure (CPAP) therapy is the gold-standard treatment for obstructive sleep apnea (OSA). This non-invasive therapy involves the use of a machine that delivers a steady stream of air through a mask worn over the nose and/or mouth during sleep.
The CPAP device works by maintaining a consistent positive pressure within the airway, preventing it from collapsing and obstructing breathing during sleep. This continuous airflow helps keep the airways open, allowing for uninterrupted breathing and improved oxygen levels throughout the night.
CPAP therapy is highly effective in treating the symptoms of OSA, including:
- Reducing or eliminating snoring
- Improving sleep quality and reducing daytime fatigue
- Lowering the risk of associated health complications, such as heart disease and stroke
B. Effectiveness and Compliance Rates in Sleep Apnea Treatment
Numerous studies have demonstrated the effectiveness of CPAP therapy in treating OSA:
- Improvements in Breathing Interruptions:
- CPAP has been shown to significantly reduce the number of breathing pauses (apneas) and reductions in airflow (hypopneas) during sleep.
- In clinical trials, CPAP has been found to reduce the apnea-hypopnea index (AHI), a measure of the severity of sleep apnea, by 70-90% in most patients.
- Enhanced Oxygen Levels:
- CPAP therapy helps maintain adequate oxygen levels in the blood by keeping the airways open and improving ventilation during sleep.
- Studies have reported significant improvements in oxygen saturation levels in patients using CPAP compared to those with untreated OSA.
Despite the proven effectiveness of CPAP, long-term compliance with the therapy can be a challenge for some patients. Factors that can influence CPAP compliance include:
- Mask Comfort and Fit:
- Proper fitting and comfort of the CPAP mask are crucial for patient acceptance and adherence to the therapy.
- Mask-related issues, such as air leaks or skin irritation, can lead to poor compliance.
- Side Effects:
- Some patients may experience side effects like dry mouth, nasal congestion, or skin irritation, which can make CPAP use uncomfortable.
- Addressing these side effects through humidification, nasal sprays, or mask adjustments can help improve compliance.
By addressing these factors and providing comprehensive care, healthcare providers can work to optimize CPAP adherence and ensure that patients with OSA receive the full benefits of this highly effective treatment.
CPAP Therapy for Obstructive Sleep Apnea
A. Overview of Continuous Positive Airway Pressure (CPAP) Therapy
As mentioned earlier, CPAP is the gold-standard treatment for OSA. It works by delivering a steady, gentle flow of air through a mask worn over the nose and/or mouth during sleep. This positive airway pressure helps keep the airway open, preventing it from collapsing and obstructing breathing.
The CPAP device consists of three main components:
- The CPAP machine: This generates the steady flow of air at the prescribed pressure level.
- The CPAP mask: This is worn over the nose, mouth, or both, and is connected to the air hose.
- The air hose: This connects the CPAP machine to the mask, delivering the pressurized air.
CPAP therapy has been shown to be highly effective in treating the symptoms of OSA, including:
- Reducing or eliminating snoring
- Improving sleep quality and reducing daytime fatigue
- Lowering the risk of associated health complications, such as heart disease and stroke
B. Effectiveness and Compliance Rates in Sleep Apnea Treatment
The effectiveness of CPAP therapy has been extensively studied, and the results are quite compelling:
- Reduction in Breathing Interruptions:
- Studies have consistently shown that CPAP can reduce the apnea-hypopnea index (AHI), a measure of the severity of sleep apnea, by 70-90% in most patients.
- This significant reduction in breathing interruptions during sleep leads to improved oxygenation and better overall sleep quality.
- Improved Oxygen Levels:
- CPAP therapy helps maintain adequate oxygen levels in the blood by keeping the airways open and improving ventilation during sleep.
- Clinical trials have reported significant improvements in oxygen saturation levels in patients using CPAP compared to those with untreated OSA.
- Enhanced Sleep Quality and Daytime Function:
- CPAP has been shown to improve sleep quality by reducing sleep fragmentation and allowing patients to reach the deeper, more restorative stages of sleep.
- Patients using CPAP often report improvements in daytime alertness, energy levels, and overall quality of life.
However, the long-term success of CPAP therapy is heavily dependent on patient compliance. Factors that can influence CPAP compliance include:
- Mask Comfort and Fit:
- Proper fitting and comfort of the CPAP mask are crucial for patient acceptance and adherence to the therapy.
- Mask-related issues, such as air leaks or skin irritation, can lead to poor compliance.
- Side Effects:
- Some patients may experience side effects like dry mouth, nasal congestion, or skin irritation, which can make CPAP use uncomfortable.
- Addressing these side effects through humidification, nasal sprays, or mask adjustments can help improve compliance.
By addressing these factors and providing comprehensive care, healthcare providers can work to optimize CPAP adherence and ensure that patients with OSA receive the full benefits of this highly effective treatment.
When to Talk to Your Doctor About Snoring
A. Recognizing When Snoring Warrants Medical Attention
While occasional snoring is common and not necessarily a cause for concern, there are certain situations where snoring may be a sign of a more serious underlying issue that requires medical attention:
- Persistent or Loud Snoring:
- If snoring is a regular occurrence, occurring several nights a week or lasting for prolonged periods, it’s worth discussing with a healthcare provider.
- Pauses in Breathing:
- If you or a bed partner notice that the snoring is interrupted by periods of silence, followed by gasping or choking sounds, this could be a sign of sleep apnea and should be evaluated.
- Daytime Fatigue and Sleepiness:
- Excessive daytime sleepiness, difficulty concentrating, or feeling unrested despite adequate sleep time may indicate an underlying sleep disorder.
B. Seeking Professional Guidance for Sleep-related Concerns
If you or your healthcare provider recognize any of the above signs, it’s important to consult with a sleep specialist or otolaryngologist (ENT doctor) for a comprehensive evaluation:
- Sleep Study (Polysomnography):
- This overnight sleep study in a sleep laboratory can provide a detailed assessment of your sleep patterns, breathing, and oxygen levels, helping to diagnose any underlying sleep disorders.
- Physical Examination:
- Your healthcare provider will perform a thorough physical examination, including an assessment of your airway, nasal passages, and throat, to identify potential anatomical factors contributing to your snoring.
- Risk Factor Assessment:
- Your doctor will review your medical history, lifestyle factors, and any other conditions that may be influencing your sleep quality and snoring.
- Personalized Treatment Plan:
- Based on the findings from the evaluation, your healthcare provider will work with you to develop a customized treatment plan to address the underlying causes of your snoring and improve your sleep health.
Seeking professional guidance is crucial, as untreated sleep-related issues can have significant consequences on your overall health and quality of life. By taking proactive steps to address snoring and other sleep concerns, you can take the first steps towards better sleep and improved wellbeing.
Conclusion
A. Taking Steps Towards Better Sleep and Overall Health
Snoring and sleep-related disorders can have far-reaching impacts on an individual’s physical and mental health. By recognizing the signs that warrant medical attention, seeking professional guidance, and implementing appropriate treatment strategies, individuals can take proactive steps towards achieving better sleep and improved overall health.
B. Importance of Early Detection and Intervention
Early detection and intervention are key when it comes to addressing sleep-related issues. Untreated conditions like obstructive sleep apnea can increase the risk of developing serious health complications, such as cardiovascular disease, stroke, and metabolic disorders.
By addressing snoring and other sleep-related concerns promptly, individuals can mitigate these risks and enjoy the benefits of better sleep and overall wellbeing.
Remember, your health and sleep quality are vitally important. Don’t hesitate to have an open and honest conversation with your healthcare provider about any sleep-related concerns you may have. Together, you can develop a comprehensive plan to help you achieve the restful, restorative sleep you deserve.

